This article reviews emerging evidence connecting gut microbiota to scalp health and hair growth. We synthesize recent findings from microbiome and dermatology research to explain how gut-derived immune signals, microbial metabolites like short-chain fatty acids, and systemic inflammation may influence scalp inflammation and hair follicle cycling. The goal is to present an academically rigorous but practical framework for health-conscious readers considering integrative strategies to support hair from the inside out.
Understanding the gut‑scalp connection: microbiome and immunity

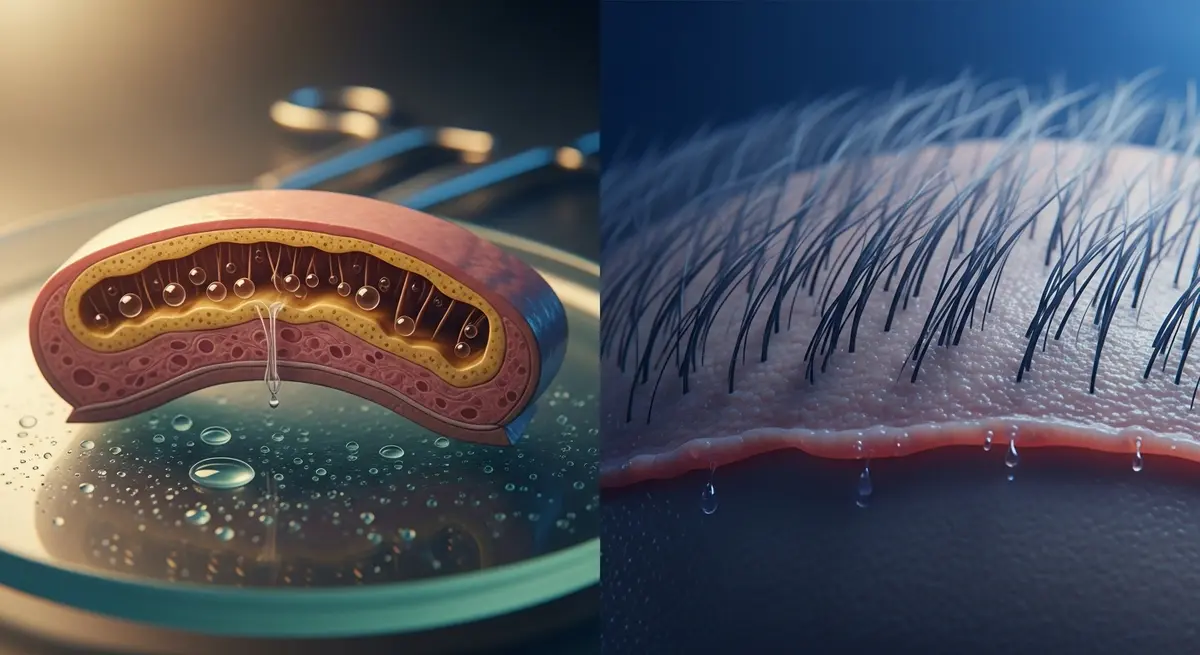
The relationship between the gut microbiome and scalp health is increasingly recognized as a biologically plausible pathway linking digestion, systemic immunity, and hair follicle biology. At its core are two related concepts often discussed in current dermatology and microbiome literature: the gut–skin axis and the more specific gut–hair axis. These frameworks propose that microbial communities in the intestine influence distant tissues through metabolites, immune signaling, and effects on epithelial barrier integrity (Journal of Investigative Dermatology; Gut; Nature Reviews Microbiology).
Fundamental terminology clarifies the mechanisms discussed here. Dysbiosis denotes a shift in the composition or function of microbial communities away from a state associated with health. Barrier function refers to the intestinal epithelium’s ability to restrict translocation of microbes and microbial products into the circulation. Cytokines are signaling proteins (for example, IL‑1β, IL‑6, TNF‑α, IFN‑γ) released by immune cells that orchestrate inflammation and can act locally or systemically.
How might gut-derived processes influence the scalp? Several converging pathways are supported by preclinical and translational data. First, microbial metabolites — notably short‑chain fatty acids (SCFAs) such as butyrate and propionate — modulate systemic immune tone and regulatory T‑cell function. SCFAs are anti‑inflammatory in many contexts and help maintain epithelial barrier integrity; their reduction during dysbiosis can favor pro‑inflammatory states that extend beyond the gut (Nature Reviews Microbiology; Frontiers in Immunology).
Second, intestinal barrier disruption (often termed “increased intestinal permeability”) permits translocation of microbe‑associated molecular patterns such as lipopolysaccharide (LPS). LPS is a potent activator of innate immunity and can drive systemic production of IL‑6 and TNF‑α, cytokines implicated in scalp inflammation and hair follicle cycling disturbances (Gut; Journal of Dermatological Science). Persistent, low‑grade systemic inflammation—measured in some studies by elevated circulating cytokines or acute‑phase proteins—can sensitize skin and follicular immune environments to local triggers.
Third, immune cell trafficking provides a cellular bridge. Dysbiosis can skew T‑cell subsets (for example, toward Th17 or Th1 phenotypes) and expand populations of effector cells that recirculate and home to peripheral tissues, including skin and hair follicles. Inflammatory T‑cell infiltrates around the follicle are a hallmark of many inflammation‑driven hair disorders and can shift hair follicles from anagen (growth) into catagen or telogen (involution or shedding) prematurely (Journal of Investigative Dermatology; Experimental Dermatology).
These mechanisms help explain clinical observations linking gut disturbances to scalp conditions. For example, inflammatory scalp diseases such as seborrheic dermatitis, psoriasis, and certain forms of alopecia (including alopecia areata and telogen effluvium when associated with systemic illness) often coexist with markers of systemic immune activation. While causality is not universally proven, the pattern—microbial imbalance or reduced microbial diversity, changes in SCFA profiles, elevated circulating cytokines—forms a consistent mechanistic hypothesis explored in dermatology and microbiome journals.
Why this matters for the health‑conscious reader: understanding these pathways reframes scalp conditions not solely as local problems but as potentially systemic ones amenable to integrative strategies. Interventions that restore microbial balance, support barrier integrity, or temper systemic inflammation could complement topical and procedural dermatologic therapies. For readers seeking to deepen their grasp of how surface microbial communities integrate with these systemic dynamics, a skin microbiome primer provides helpful background on surface immunity and barrier function: skin microbiome primer.
Caveats are important. Much of the most detailed mechanistic work comes from animal models or small human cohorts; scalp‑specific, large randomized controlled trials remain limited. Nevertheless, the convergence of data from immunology, gastroenterology, and dermatology journals supports a cautious, evidence‑oriented interest in gut‑targeted adjunctive approaches for inflammation‑driven hair loss and scalp disease (Journal of Investigative Dermatology; Gut; Frontiers in Microbiology).
In summary, the gut‑scalp connection rests on clear biological principles: microbial metabolites and products shape systemic immunity, barrier dysfunction permits inflammatory mediators into circulation, and immune cell trafficking links gut‑derived signals to follicular microenvironments. Recognizing these links creates a rational platform for combined dermatologic and gut‑focused strategies, pursued under clinical guidance and with attention to the evolving evidence base.
Mechanisms: metabolites, barrier integrity, and inflammatory pathways
The gut microbiota influences distant tissues through a constellation of metabolites, translocated microbial products, and immune signals that together shape systemic inflammation and tissue-specific responses in the scalp. Short‑chain fatty acids (SCFAs) such as butyrate and propionate are among the most well‑characterized mediators: synthesized by bacterial fermentation of dietary fiber, they act locally on intestinal epithelium to strengthen barrier function and remotely on the immune system to reduce pro‑inflammatory tone. Butyrate promotes regulatory T cell (Treg) differentiation via histone deacetylase (HDAC) inhibition and supports epithelial health, while propionate and acetate engage G‑protein coupled receptors (notably GPR41/GPR43) to modulate neutrophil recruitment and cytokine output—mechanisms that lower circulating pro‑inflammatory cytokines and preserve mucosal integrity (Furusawa et al., 2013; Arpaia et al., 2013; Maslowski et al., 2009; Smith et al., 2013).
When SCFA production or signaling is reduced—commonly after dietary shifts or dysbiosis—the intestinal barrier can weaken. Increased intestinal permeability permits passage of microbial components such as lipopolysaccharide (LPS) into the portal and systemic circulation, a state often described as metabolic endotoxemia. Circulating LPS binds toll‑like receptor 4 (TLR4) on innate immune cells and parenchymal tissues, triggering NF‑κB dependent transcription and release of IL‑1β, IL‑6 and TNF‑α; these cytokines are central drivers of low‑grade systemic inflammation and oxidative stress (Cani et al., 2007; Cani et al., 2008). Preclinical models show that diet‑induced increases in gut permeability and LPS translocation elevate systemic IL‑6 and TNF‑α and raise markers of reactive oxygen species (ROS) production, linking barrier dysfunction to a pro‑oxidant, pro‑inflammatory milieu (Membrez et al., 2008; Creely et al., 2007).
Systemic cytokines and oxidative stress reach the scalp via the circulation and can alter hair follicle biology in several mechanistic ways. Hair follicles are dynamic mini‑organs with tightly regulated cycling through anagen (growth), catagen (regression) and telogen (rest). Pro‑inflammatory cytokines—including IL‑1β, IL‑6 and TNF‑α—directly perturb this cycle: experimental work demonstrates that IL‑1β and TNF‑α induce premature catagen entry and suppress anagen maintenance, in part by antagonizing Wnt/β‑catenin signaling and activating apoptotic or regression programs within follicular keratinocytes (Ito et al., 2004; Paus et al., 1997; Kwack et al., 2011). Elevated IL‑6 also correlates with impaired follicular proliferation and has been shown to inhibit hair shaft elongation in organ and animal models (Kwack et al., 2011; Hoffmann et al., 2010).
Oxidative stress compounds these effects: ROS can damage follicular stem cells and dermal papilla cells, impairing their capacity to support anagen. Chronic, low‑grade oxidant exposure shifts the local redox balance and can sensitize follicles to cytokine‑induced regression, thereby translating systemic inflammatory signals into localized hair loss or thinning (Hoffmann et al., 2010).
Immune cell trafficking provides a cellular bridge between gut‑derived immune priming and scalp responses. Antigen‑presenting cells in the gut lamina propria sample microbial antigens and migrate to mesenteric lymph nodes to prime T cell populations. Gut‑educated T cells and innate immune populations can acquire tissue‑homing properties and, under certain chemokine contexts, redistribute to non‑intestinal sites including the skin and scalp. Reviews of the gut‑skin axis outline how gut dysbiosis skews T helper subsets (e.g., increases in Th17 or reductions in Treg balance) and fosters systemic cytokine profiles that favor cutaneous inflammation; these circulating immune mediators and cells then interact with resident scalp immune cells to break or alter follicular immune privilege and promote inflammatory folliculitis or catagen induction (Salem et al., 2018; Zhang et al., 2021; Park et al., 2022). The net effect is a multi‑step cascade: microbial imbalance → reduced SCFA signaling and barrier loss → LPS translocation and systemic cytokine upregulation → oxidative stress and immune cell redistribution → direct suppression of anagen and promotion of catagen.
Mechanistic studies support several intervention points where gut‑targeted strategies could plausibly influence scalp outcomes. Restoring SCFA production through dietary fiber, prebiotics, or selected probiotic strains may reinforce epithelial tight junctions and re‑establish immunoregulatory signaling (Furusawa et al., 2013; Maslowski et al., 2009). Conversely, limiting LPS translocation—by improving barrier integrity or reducing dysbiotic overgrowth—reduces TLR4‑driven systemic cytokine release and oxidative load (Cani et al., 2007). At the scalp level, reducing circulating IL‑1β, IL‑6 and TNF‑α is mechanistically consistent with preserving anagen and protecting follicular stem cell niches (Ito et al., 2004; Kwack et al., 2011).
While many mechanistic links are supported by robust preclinical work, translation to human scalp health requires targeted clinical trials. Nonetheless, the converging evidence—molecular, cellular, and animal—outlines a coherent biological route by which the gut‑microbiome ecosystem can influence scalp inflammation and hair cycle dynamics. For clinicians and wellness‑minded readers, the mechanistic picture suggests that strategies which restore SCFA‑mediated regulation, protect barrier integrity, and reduce systemic endotoxin exposure may be rational complements to direct dermatologic therapies.
References cited in this text include primary and review studies that characterize SCFA immunomodulation (Furusawa et al., 2013; Arpaia et al., 2013; Maslowski et al., 2009; Smith et al., 2013), LPS‑driven endotoxemia and cytokine induction (Cani et al., 2007; Cani et al., 2008; Membrez et al., 2008), and cytokine‑mediated disruption of hair follicle cycling (Ito et al., 2004; Paus et al., 1997; Kwack et al., 2011; Hoffmann et al., 2010), along with contemporary reviews of the gut‑skin/gut‑hair axes (Salem et al., 2018; Zhang et al., 2021; Park et al., 2022).
Clinical evidence and practical interventions: probiotics, diet, and scalp care

The last half‑decade has brought a concentrated effort to translate microbiome science into clinical strategies for inflammatory scalp disease and hair loss. Trials and translational studies published between 2020 and 2025 emphasize mechanistic plausibility—short‑chain fatty acids (SCFAs), microbial regulation of intestinal barrier function, and reduced endotoxin translocation—as mediators that could modulate scalp inflammation and hair‑follicle cycling. Evidence strength varies: several rigorous preclinical studies and small controlled human trials suggest benefit from targeted probiotic strains and dietary patterns, but high‑quality, scalp‑focused randomized controlled trials remain limited in number and size (Journal of Investigative Dermatology; Gut Microbes; JAMA Dermatology; British Journal of Dermatology).
Clinical and translational signals
Animal models and mechanistic human studies have clarified pathways by which gut modulation can influence the scalp: increased SCFA production (notably butyrate and propionate) correlates with regulatory T‑cell induction and lower proinflammatory cytokine expression; reduced lipopolysaccharide (LPS) translocation across a healthier intestinal barrier lowers systemic innate immune activation. Translational work has identified shifts in gut taxa (for example, increases in Akkermansia and bifidobacterial groups) that accompany anti‑inflammatory effects relevant to hair follicle homeostasis. A number of probiotic preparations have shown hair‑related or anti‑inflammatory effects in small clinical series or in animal studies, supporting the concept that targeted gut interventions can be adjuvant therapies to dermatologic care.
Probiotic strains and the evidence base
Available evidence is strain‑dependent and should be interpreted conservatively. Notable strains and genera that recur across recent literature include Lactobacillus/Lacticaseibacillus (e.g., L. rhamnosus GG, L. plantarum, certain L. paracasei isolates) and Bifidobacterium species (e.g., B. longum). Preclinical work with selected Lacticaseibacillus paracasei isolates has demonstrated activation of hair‑growth pathways (Wnt/β‑catenin) in animal models and favorable shifts in gut community structure; human trials focusing directly on scalp endpoints are fewer but suggest reductions in inflammatory biomarkers and symptomatic improvement when probiotics are used adjunctively.
Practical considerations when selecting probiotics
- Prioritize products that list strain designations (not just genus/species) and have human data supporting the specific strain for immune or skin outcomes.
- Therapeutic dosing in trials varies; many interventions use daily doses in the range of 1 × 10^9 to 1 × 10^10 CFU for single strains, while multi‑strain products and some trials use higher total CFU counts. Clinically, expect to trial a product for at least 8–12 weeks before judging effect.
- Choose well‑manufactured formulations (cold chain or demonstrated shelf stability) from reputable manufacturers; confirm exclusion criteria for immunocompromised patients.
Dietary and prebiotic strategies
Dietary patterns that increase fermentable fiber and polyphenol availability reliably support SCFA‑producing taxa. Mediterranean‑style patterns—emphasizing vegetables, legumes, whole grains, olive oil, nuts, and moderate fish—consistently correlate with lower systemic inflammation and greater microbial diversity in cohort studies and interventional work. Practical dietary guidance includes increasing soluble and insoluble fiber (targeting individualized goals commonly between 20–35 g/day depending on tolerance), prioritizing whole‑food polyphenol sources (berries, green tea, extra‑virgin olive oil), and including fermented foods (yogurt, kefir, certain fermented vegetables) as tolerated.
Prebiotics (inulin, fructooligosaccharides, partially hydrolyzed guar gum) can selectively stimulate bifidobacteria and SCFA production; however, dosing should be individualized because fermentable substrates can exacerbate symptoms in patients with significant gut sensitivity.
Limits of current trials and research gaps
- Heterogeneous endpoints: many studies measure surrogate biomarkers (cytokines, fecal metabolites) rather than standardized scalp outcomes (hair count, photographic global assessment, trichoscopy). That complicates translation into practice.
- Small sample sizes and short durations: several randomized studies are underpowered for clinically meaningful hair endpoints and often last <12 weeks.
- Strain and formulation variability: outcomes from one probiotic strain do not generalize to others; many commercial products lack the specific strains used in trials.
- Confounding interventions: concurrent topical or systemic dermatologic treatments are common in trial populations, making isolation of probiotic/dietary effects difficult.
Actionable guidance for clinicians and health‑conscious readers
Clinical framework for integrating gut‑targeted care into scalp management:
- Baseline assessment
- Document scalp diagnosis and severity with standardized measures (photography, trichoscopy, global severity scales). Obtain baseline labs relevant to hair loss and inflammation: CBC, ferritin, TSH, 25‑OH vitamin D, fasting glucose/HbA1c as indicated, CRP. In patients with GI symptoms, consider fecal calprotectin or referral for gastroenterology.
- Treatment selection and monitoring
- When recommending probiotics: select preparations that specify strain(s) and have supporting human or strong translational data for immune modulation. Discuss realistic expectations: adjunctive, modest effects over months rather than immediate hair regrowth.
- Duration and reassessment: a pragmatic trial of 12 weeks is reasonable for initial assessment; extend to 6 months if tolerability and partial benefit are observed. Reassess clinical endpoints and inflammatory markers (CRP, symptom scales) at intervals.
- Safety screening: avoid live probiotics in patients with severe immunosuppression or central venous access. Monitor for uncommon adverse events (GI upset, rare bacteremia).
- Dietary counseling
- Encourage a Mediterranean‑style pattern, individualized fiber increases, and regular intake of anti‑inflammatory fats (olive oil, omega‑3‑rich fish). Reduce ultra‑processed foods and excessive simple sugars that promote dysbiosis.
- Use prebiotics cautiously in patients with bloating/functional gut disorders; consider starting low and titrating.
- Integrating topical scalp care with systemic approaches
- Coordinate with dermatologic treatments rather than replacing them. For inflammatory scalp disease, systemic gut‑focused measures are complementary to topical anti‑inflammatories (e.g., medicated shampoos, topical corticosteroids or calcineurin inhibitors where indicated) and procedural or systemic dermatologic therapies.
- Encourage scalp barrier health: gentle, pH‑appropriate cleansers, avoidance of irritant fragrances or harsh surfactants, and attention to contact allergens. For patients with seborrheic dermatitis or dermatitis‑driven shedding, adding antifungal agents (e.g., topical ketoconazole) or anti‑inflammatory topicals can address local drivers while the systemic plan is implemented.
- Outcome measurement and when to escalate
- Use objective measures where possible (hair counts from vertex fields, standardized photography, validated symptom scales). If no clinical improvement after 6 months of combined topical and gut‑targeted strategies, escalate to specialty dermatology interventions or consider referral for immunologic or nutritional evaluation.
Practical patient messaging
- Emphasize that gut‑targeted interventions are supportive and best used as part of a comprehensive plan. Risks are generally low for healthy adults, but benefits are incremental and vary by individual.
- Encourage evidence‑based lifestyle changes (dietary pattern, reduced smoking, sleep, stress reduction) that synergize with any probiotic or prebiotic strategy.
Research priorities and closing perspective
To move from plausibility to practice, the field needs larger, strain‑specific randomized controlled trials with standardized scalp endpoints, longer follow‑up, and clear reporting of concomitant therapies. Biomarker work (SCFA panels, cytokine profiling, validated intestinal permeability measures) will help identify mechanistic responders and refine personalized approaches. For now, clinicians and informed readers can reasonably incorporate carefully selected probiotics and Mediterranean‑style diet changes as adjunctive measures while prioritizing established dermatologic therapies for inflammation‑driven hair loss.
The evolving literature—anchored in dermatology and microbiome journals—supports a complementary role for gut‑focused interventions. Thoughtful selection of probiotic strains, structured dietary changes, and careful coordination with topical scalp care offer a practical, biologically informed path for individuals seeking integrative care for scalp inflammation and hair loss.
Conclusion
Current research supports a biologically plausible link between gut microbiota and scalp inflammation, with mechanisms spanning immune modulation, microbial metabolites, and barrier dysfunction. While preclinical and small clinical studies are promising—particularly for specific probiotic strains—high-quality, scalp-focused trials remain limited. Readers should view gut-targeted strategies as complementary to dermatologic care, pursuing evidence-based dietary and probiotic approaches in consultation with clinicians.
Ready to support your scalp from the inside out? Learn about internal hair care at internal hair care.



